Overlooked solutions to lessen the brunt of COVID crisis in India
Please click here to read the full FTC Affiliate Disclosure policy.
- August 27, 2024 @ 20:02 pm EDT
- comments
Like everyone else, I sit here, appalled at the picture emerging out of India. The new specter of fungal infections makes an already awful situation incrementally worse. As someone with a Ph.D. in immunology, it strikes me that simple, inexpensive things that may help are being overlooked; this post is to talk about that.
Fixing Vitamin D deficiency
There have been a whole host of studies showing that patients with lower vitamin D levels are more susceptible to having a more severe disease course, and dying from COVID – this has also been shown in the Indian population.
There are very conflicting data on whether giving vitamin D after you get COVID is helpful at all – it may be akin to shutting the barn door after the horse has bolted, because of the myriad roles vitamin D plays. The smarter thing to do is to get your Vitamin D levels into the normal range (30 ng/mL or higher) BEFORE you come into contact with the virus.
About 50-90% of the Indian population is vitamin D deficient, with most studies showing 80-90% deficiency. So when India is in the throes of a horrifying pandemic with ridiculous morbidity and mortality, why is the Indian population not being told loud and clear to get their vitamin D levels checked, and supplement accordingly before they get infected with the virus? Or at least supplement to a degree without checking?
Before I started researching this blog post, I was optimistically assuming that the vitamin D message had been spread to a good degree across India. I ran a quick poll in the group of largely Indian expats I run – when I asked them to check with families in India whether they were aware of their vitamin D level and were supplementing, see the results below – almost half were unaware.
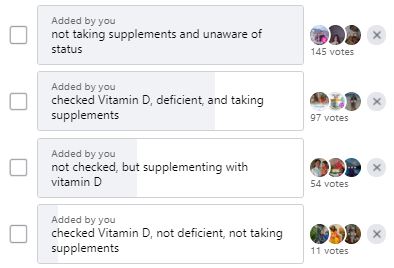
If this is the case in well-educated families with better access to healthcare, what is the case among the less educated in the more rural areas? Public education on this topic should happen, and will likely save lives if it does.
Use of nutraceuticals such as turmeric in the treatment regimen
People familiar with the vast body of research (over 16000 articles on PubMed) on curcumin, the principal active ingredient of turmeric, are aware that it could, in theory, help with the COVID infection course in so many ways. Similar to steroids and vitamin D, it suppresses the production of inflammatory cytokines. While steroids are only immunosuppressive, turmeric is also anti-viral, demonstrating anti-viral activity against a plethora of viruses through a vast variety of mechanisms. In the case of SARS-CoV2, the causative agent of COVID, a computational analysis also revealed mechanisms by which curcumin may be protective.
Despite all this, there has been a tremendous, almost incomprehensible resistance to even investigating the effect of nutraceuticals such as turmeric in COVID, making any sort of conclusion hard to draw. There was finally a study by a doctor in Maharashtra examining either conventional treatments alone, or conventional treatments plus curcumin in COVID – this study showed that giving curcumin with conventional treatment regimens resulted in significant improvements – interestingly, the combination allowed patients to maintain oxygen saturation better on room air, which is literally the overwhelming need of the hour. This paper, which is provisionally accepted by Frontiers in Pharmacology, should be available in full form soon.
But this is one doctor open to trying this for her patients- most doctors are still only using the conventional treatments alone, with poorer outcomes, if this study is to be believed. On social media, people beg for remdesivir or tocilizumab, while ingredients sitting in their own pantry, in medicinal doses, may replicate some of the results these drugs achieve- for example, anti-viral and IL-6 suppressive activity. Most patients don’t even have access to a hospital, and self-care is the only option left to them. If they took turmeric alone instead of taking nothing, their outcomes may conceivably be better, though obviously, no conclusions can be drawn given the lack of studies about curcumin alone in COVID. Nonetheless, it is both cheap and safe, so worth a try, especially when the stakes are so high.
How to take turmeric: Turmeric/curcumin is notoriously poorly absorbed and assimilated. Your best bet to improving absorption is mixing it with coconut oil and black pepper (to provide piperine, which helps the body retain the absorbed turmeric). Here is a good turmeric homebrew: Mix 2 tsp of turmeric with cold-pressed or virgin coconut oil, and add 1/4 tsp of black pepper – the resulting paste can be mixed with honey and directly eaten, or taken in milk. I would do this 2-3 times a day.
Taking too much turmeric is also not good for you: side effects of excessive turmeric consumption include allergic reactions, diarrhea, constipation, abdominal pain, nausea and vomiting. It can also interfere with certain medications – please discuss with your doctor before taking it – this is a good resource to share with your doc if you want to have that conversation.
Taking probiotics with antibiotics to prevent the development of mucormycosis (black fungus)
In most cases, patients are being given antibiotics that will wipe out all the good bacteria in their gut, while also sometimes concurrently being prescribed immunosuppressive medications, and while also breathing in oxygen from dirty unsanitized equipment. It is quite literally the perfect storm to create an epidemic of black fungus.
One really simple safeguard against this – prevent the field from being wiped out by antibiotics. Take probiotics with your antibiotics! This is always a sound strategy; I also cannot survive antibiotics without probiotics – the side effects are too debilitating for me. A good probiotic option in this situation is probably Enterogermina (antibiotic-resistant Bacillus claussii) available at all pharmacies in India. I don’t think it needs a prescription, but check with your doctor about the probiotics as well, and see if they suggest any alternatives. Once you are off antibiotics, take plenty of yogurt (you can also do this while on antibiotics, but may not be as effective).
Another thing that may help – taking turmeric. It also has anti-fungal activity against various species – I have not been able to determine if its anti-fungal activity extends to mucormycetes – but it’s possible it is effective to some degree here.
All of these ideas are my inferences based on what is published, and I will remind people that I have no medical degree, only a PhD in immunology and an inquiring mind. Any suggestions in here should be carried out in consultation with a medical doctor.
General disclaimer: This blog provides general information and serves as a forum for discussing about medicine and health in the context of the latest studies. The words and other content provided in this blog, and in any linked materials, are not intended and should not be construed as medical advice. If the reader or any other person has a medical concern, he or she should consult with an appropriately-licensed physician or other health care worker. Never disregard professional medical advice or delay in seeking it because of something you have read on this blog or in any linked materials. If you think you may have a medical emergency, call your doctor or an emergency number immediately. The views expressed on this blog and website have no relation to those of any academic, hospital, practice or other institution with which the authors are affiliated.















